Surgical claims most delayed under SHA payment system—study

Fresh analysis shows that a huge proportion of surgical all claims in Kenya's healthcare system remain in prolonged review by the Social Health Authority (SHA) officials.
Over half of insurance payment claims on surgery procedures lodged under the Social Health Authority (SHA) went unprocessed for three consecutive months, underscoring the persistent delays in honoring medical bills that continues to hurt the healthcare system.
These startling revelation is contained in a new study by the Rural and Urban Private Hospitals Association of Kenya (RUPHA), which notes that this payment challenge stifled operations among private and faith-backed hospitals offering "high-tier services" to patients across Kenya during the period under focus.
"While only a third of Social Health Insurance Fund (SHIF) claims were surgical, 39 percent of facilities identified surgical claims as the most problematic, pointing to high claim value and complexity," the RUPHA study, which was undertaken between 23rd April and 6th May this year states in part.
The survey is part of a continuous monitoring initiative launched at the start of Kenya’s transition from the National Health Insurance Fund (NHIF) to SHA under President William Ruto.
A total of 477 healthcare facilities across all levels of care and ownership types—including public, private, and faith-based institutions participated in the study that sought to lift the veil on the latest status of SHA contracting, Primary Health Care (PHC) accreditation, reimbursement patterns, claim bottlenecks, and the underlying financial health of healthcare facilities.
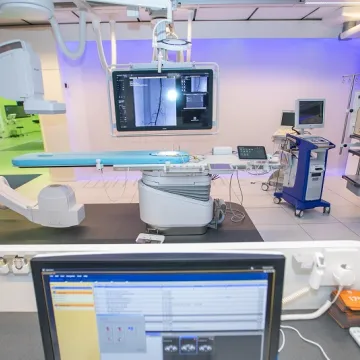
Out of the Level 3–5 healthcare facilities that were surveyed, 33 percent noted that surgical procedures accounted for over 30 percent of their submitted claims while 20 percent said that more than half of all claims lodged with SHA were surgical in nature. At Level 5, surgical claims increased to 67 percent, reflecting these centres' role as surgical referral institutions.
Analysis shows that a significant proportion of surgical all claims in the country's healthcare system remain in prolonged review by the authorities. For instance, nearly four out of 10 or 39 percent of hospitals reported that over 50 percent of their surgical claims were still under review by SHA for a long period of time.
"Another 19 percent indicated that 30–50 percent of their surgical claims were pending review. Only 15 percent reported that all surgical claims had been processed and cleared."
Additionally, the study singled out faith-based hospitals, noting that without timely payments, these facilities would be at huge financial pressure given that they serve a "significant referral and surgical care role. At the moment, faith-based hospitals and healthcare facilities are struggling due to high exposure to "NHIF arrears, unpredictable PHC reimbursements, and slower SHIF settlements."
While surgical claims top the list of problematic pending payments at 39 percent, the survey shows that other challenging claim categories were inpatient medical claims at 28 percent, outpatient SHIF claims at 19 percent and maternity claims at 14 percent.
"The dominance of surgical claims as a bottleneck reflects the complexity, higher value, and documentation intensity of these claims—factors that often result in extended review periods and disputes," the study explains in part.
To counter the challenges bedeviling the delayed payment of surgical claims, the study recommended that the Ministry of Health established a dedicated processing lane and verification protocols for surgical claims "to avoid collapse of high-cost services."
The specter of delayed payments on surgical procedures was also reported across the government-backed healthcare system that runs under Level I to Level VI tier of hospitals.
For instance, while 89 percent of Level 3 facilities said they had no surgical claims under review, nearly half or 47 percent of facilities reported that more than half of their surgical claims were yet to be settled.
"These trends suggest that the higher the level of care—and the greater the surgical load— the more likely it is that surgical claims remain stuck in the SHA review pipeline," RUPHA report said.